Think it's plantar fasciitis? Think Again...
Mar 05, 2024
AND... by the way...Stop Stretching Your Hamstrings!
The title and the above statement may have got your attention…as they should. Strangely enough, what you may feel in the back of your thigh and your "plantar fasciitis" may be related. If this sounds odd, let me illustrate the bigger picture along with a quick background of my experience.
When I first graduated from physical therapy school, this lifelong runner was excited to simply get back out to run the roads and trails he loved without the stress of taking the next test. And, of course, I would stretch afterward; primarily my hamstrings. It is the easiest to target. Just sit down and put your leg out in front of you. They can often feel tight, too…can’t they? I mean, do they always have to feel tight? Like…ALL THE TIME. Or is it really JUST the hamstrings back there? Well…no.
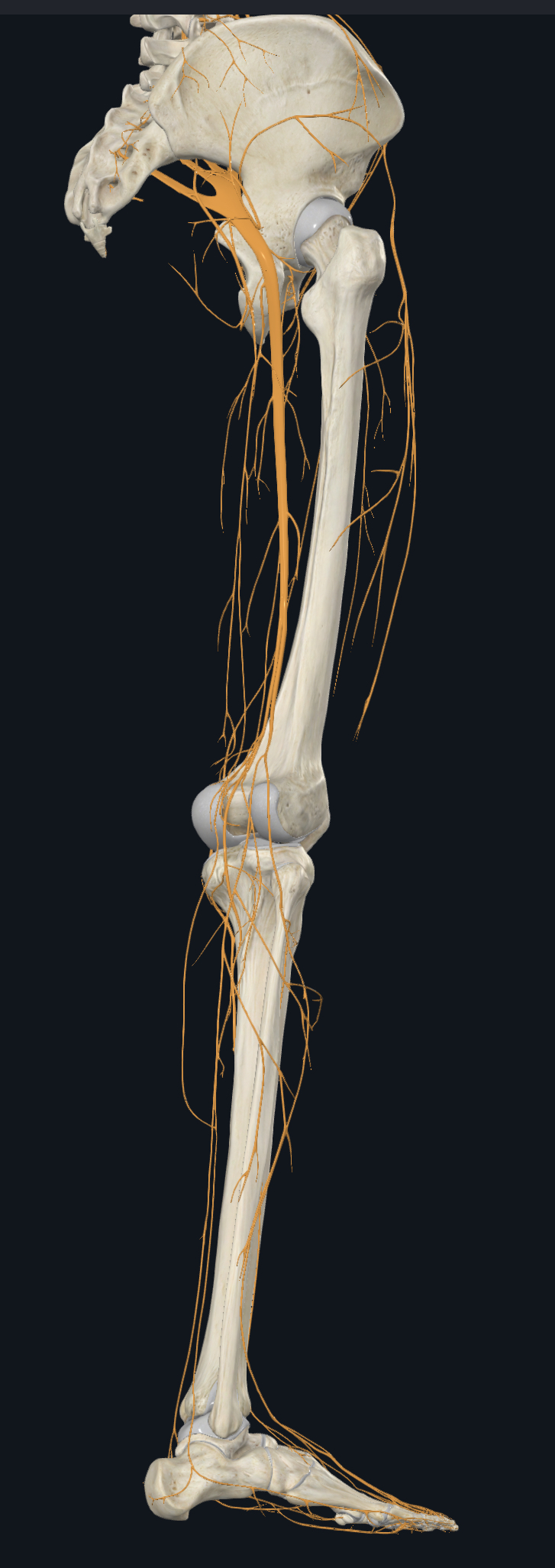
When I started to stretch my hamstrings, I noticed the “stretch” in the back of my KNEE and in my CALF. Being, fresh out of PT school I knew I wasn’t stretching my calf. I was stretching my hamstring but felt it a bit in my calf and the back of my knee. I knew this was the nervous system I was feeling. And I think we may all know how to stretch our calves and it was completely different from what I was doing. When I was stretching, the sciatic nerve and its branches as they go down the back of the leg were getting put under tension, along with my hamstrings. Being fresh out of PT school I thought, “I know what to do about this".
I immediately used a technique that mobilizes the nervous system with the hope of it gaining the ability to move better in the back of my thigh. Well unbeknownst to me, after doing this at the end of my run for just three days, I was too aggressive because my per mile time for my typical six-miler went from 7:30 pace to 20:00!! Because I now felt zinging/aching down the back of my legs…every time I took a stride. So to get at least as good of a workout I now had to almost hop vertically a bit from foot to foot. You can imagine how I looked on my “run”! But it felt awful to take that zinging down my leg if I took a normal stride. This was a problem for quite some time.
The moral of the story is if you feel it in your CALF or the back of your knee when you are stretching your hamstring, you ARE likely STRETCHING YOUR SCIATIC NERVE. This problem led me to a lifelong professional concentration on discovering how the nerves…all on their own…can be the problem and apply this to running injuries. What I am saying is the problem is NOT always a tendon, ligament, muscle, etc. It can often be a MASQUERADE from irritation of the nerves in the area. In this case the area of the plantar fascia. And the lower back can feel fine and have NOTHING wrong with it. Who would have thought…the nerves in the legs (and arms) could be the real problem?
I’ve seen much more of this recently since the pandemic. The combination of less activity, more sitting, and more stress all come together to make it much easier for the nerves to cause pain or discomfort. This is likely much more of a widespread issue than you think…or even your physiotherapist, chiropractor, or physician think. And just because the MRI finds something…DOESN’T always mean what is “found” on the MRI is the problem. What is seen on the MRI may NOT be the problem.
In the leg, I have seen the sciatic nerve masquerade as a problem with the IT band, hamstring (and upper hamstring), and tight hips. I’ve seen the saphenous nerve masquerade as an MCL (medial collateral ligament) issue, pes anserine bursitis, medial plica issue, and shin splints. I’ve seen the infra-patellar branch of the saphenous nerve (IBSN) masquerade as a meniscal problem, infra-patellar tendinitis, runner’s knee (chondromalacia or Patellofemoral pain syndrome), jumper’s knee, and quadriceps tendinitis…just to name a few. This local nerve pain can be masquerading as a typical musculoskeletal problem just about everywhere. After all, everything has a nerve supply…and that nerve supply or the nerve running next to the structure that hurts can be a pain generator, all on its own, unrelated to a problem in the spine.
This opens up a can of worms a bit, doesn’t it? Yep. It does. But at least now we know.
As crazy, and complicated as it sounds, it possibly brings some clarity as to why sometimes NOBODY knows what is going on with your injury or why you may know somebody who had surgery. But, unfortunately, it didn’t help.
Well, today we won’t solve all of these problems. But we will bring clarity to one of the most common problems runners (and non-runners alike) often suffer from; Plantar Fasciitis. We will also discuss how the often overlooked nerves on the bottom of the heel can cause this pain and some quick tips for what to do about it.
The problem with overcoming plantar fasciitis (even without nerves being involved as pain generators) is that there is NO WAY to be on our feet and go anywhere without putting pressure on the thing that hurts. About 60% of our body weight is on our heels. Regardless of our total body weight, THAT is a tall order to be handled by this small surface area. Particularly when it hurts! It is designed to take this pressure, but when we have paved EVERYTHING like sidewalks, roads, hardwood floors, cement slab foundations for work or our home, as well as so much artificial turf that virtually nothing we stand or walk on anymore is the natural earth (sand, dirt, grass, etc). We can talk all we want about getting a stronger arch, foot, and lower leg, but it's the surfaces that we spend so much time on that are the primary issue.
And love them or hate them, this is why very cushioned rocker-bottom shoes often help (HOKA for example, etc.). Whenever the foot hits the ground, the body must respond and absorb the shock. This shoe design with its cushion and a rocker-bottom helps to make that response less abrupt and more like a dimmer switch you can more slowly turn on and turn off. There is less stress on most structures this way.
Whatever your foot may look like, high arch, normal arch, or low arch, if you have true plantar fasciitis you will benefit from something under your arch. For the plantar fascia at the bottom of your heel to feel better, the pressure of your body weight must be distributed by more surface area under your foot instead of just your heel and ball of the foot. In other words, your heel needs some help…more support. Not harsh support either. The arch support needs to be firm but forgiving. There is a lot to talk about regarding all of the things that help this structure feel better. However, minimizing pressure and pulling force to the plantar fascia on the bottom of the heel plays a vital role in allowing this structure to feel better. This is the foundation of the healing process for any structure, including irritated nerves down the legs. This may be best discussed or taught via a video series, which I have created. However, we will now turn to the most overlooked reason; the nerves on the bottom of the heel.
It was eye-opening to me when I tested the nerves of one of my clients. He was lying down on his back on the exam table. I put his foot and ankle in a certain position, straightened his knee, and then lifted his leg by allowing only his hip to move (this is called a modified straight leg raise test). This caused pain to the bottom of his heel! I then kept his foot, ankle, and knee in the exact same position and lowered his leg back down to the table. His heel pain went away! Then I repeated this and the same thing happened. There is nothing that generates pain that extends this length from the hip to the heel except a nerve. Now if movement at the hip the way I did it causes pain at the heel, then the nerves must be involved and must be addressed (nothing else spans that distance). They need to be addressed as one structure that spans the length of the entire lower extremity. Don’t worry. This is easier than it sounds.
To make the nerves down the leg feel better, we simply can’t lie down on the side that hurts. When we sit down, we will benefit from scooting our bottom forward on the chair just a little bit so we are sitting more on our tailbone (like we are slightly reclined) instead of putting direct pressure on our glutes. To further lessen pressure on the sciatic nerve, put a small stool, wooden step, or bookbag under your foot. When you do this it will cause less pressure on the sciatic nerve as it goes down the back of your leg. Furthermore, it will not feel the "pinch" from the front edge of the chair seat. This will be more difficult in a car or truck, but some newer automobiles will allow us to move the car seat with enough variation to mimic this more pain-relieving position.
If we use an ottoman when we sit in a chair or loveseat, then our knee must stay bent when we have our foot up on it. This makes it so the nerves down the back of the leg don't endure unnecessary tension. So don’t keep your knee straight when you sit down. This also goes for when you sit in a recliner, too. Bend your knee and firmly plant your foot on the platform that swings up for your legs. If the nerve at the heel is generating the pain, then we need to make the entire nervous system down the leg feel better because it is one connected structure.


That is essentially it for a position of comfort for the nerves. They are VERY pressure-sensitive and tension-sensitive. If there is one area that hurts and there is pressure on a different nerve (albeit normal pressure from just normal sitting) that will send a signal so-to-speak to the area that actually hurts. This is how it works when nerves are irritated. Just like a badly herniated disc in the lower back putting pressure on the nerve as it exits the spine can sometimes cause pain down the leg. It’s no different if outside pressure is on other parts of the nerves in the leg (like when we are sitting or lying down). The result can be similar if the nerves on the bottom of the heel are sore. This place can also be influenced by pressure on other areas of the nervous system in the leg. The heel is designed to take lots of pressure. But, in this day and age, we have paved everything. You put pressure on the nerves in the legs in a different place (for example the sciatic nerve when you sit or lie down on it) and then the heel pain can easily get worse. It really is all “connected”. Although this may be a slightly different way to look at how it is connected.
Pressure sensitivity can be further exacerbated by a tight piriformis muscle. You may have heard of this muscle deep in your buttock area. In almost all cases, it lies over the sciatic nerve. So if this muscle could better serve the sciatic nerve (the sciatic nerve is about the size of your thumb) by being more flexible and not press so hard against the sciatic nerve, this would also be very beneficial for the heel pain that could be nerve generated.

Circling back…
I mentioned the lower back doesn’t even have to be involved in creating some of this pain or discomfort in the heel. And I mean that. However, in a few cases, it will make the heel feel better if the lower back can move easier. This can often be addressed by making the muscles in front of the lower back more flexible. That's right, the muscles in the FRONT of the lower back. They get tight from just sitting down as often as we do. So it is not difficult for these muscles to get tight and influence the flexibility of the lower back. If my clients even feel their lower back a little bit when they stretch their hip flexors, I do not recommend it.
And lastly…
There is an easy tape job to do that will also help minimize the heel pain. You just apply the tape along the nerve which is along the inside and just behind the ankle. This nerve is called the tibial nerve. If we strategically target the nerves down the leg in multiple areas when we are lying down, sitting, or standing, and utilize this tape job, then the result is what I call a “summation effect”. The consequence of this strategy is a quieting of the nervous system down the entire leg and pain relief in the heel.

If you like to know more than most doctors will ever know to STOP Plantar Fasciitis, Dr. Erik Vranesh specializes in solving running injuries and has created a detailed course designed to replace the need to see a running specialist in person! When have you ever seen a physiotherapist, chiropractor, podiatrist or physician offering a money-back guarantee? Well, right now this comprehensive course comes with a no-risk 30 day money-back guarantee!
If you no longer want to be a cash cow of the medical system that s failing you AND want to "Stop Achilles Tendinitis Now!" click the BLUE LINK BELOW to learn more about your FREE 30 day no-risk offer.
The body is designed to heal, including your Achilles Tendon. Lets start this process below, Now!

